The journey of medical diagnosis is often a complex, intricate dance between observation, expertise, and deduction. For centuries, physicians have relied on their keen intellect, vast knowledge, and clinical experience to identify diseases and guide treatment. However, as medical science advances, the sheer volume of data—from intricate imaging scans and genomic sequences to vast electronic health records—has grown exponentially, often overwhelming human capacity for comprehensive analysis. This is where Artificial Intelligence (AI) steps in, not as a replacement for human doctors, but as a powerful, indispensable partner, poised to revolutionize the very core of medical diagnosis by significantly enhancing its precision and efficiency.
- The Diagnostic Imperative: Why Precision Matters More Than Ever
- AI at the Forefront: Core Technologies Driving Diagnostic Transformation
- Machine Learning (ML): The Engine of Predictive Analytics
- Deep Learning (DL): Mimicking the Human Brain for Complex Patterns
- Natural Language Processing (NLP): Unlocking Insights from Unstructured Text
- Revolutionizing Medical Imaging: Computer Vision’s Impact
- Unlocking Insights from Data: Machine Learning in Clinical Decision Support
- AI’s Role in Analyzing Electronic Health Records (EHRs)
- Leveraging Genomic and Multi-Omics Data for Precision Diagnostics
- Integrating Wearable Device Data for Continuous Monitoring
- The Power
Imagine a future where diseases are detected earlier, misdiagnoses are drastically reduced, and treatments are tailored with unprecedented accuracy to each individual’s unique biological makeup. This future is rapidly becoming our present, thanks to the transformative power of AI in healthcare. From sophisticated algorithms that can spot minute anomalies in medical images to machine learning models that predict disease risk years in advance, AI is reshaping diagnostic pathways. This comprehensive article will delve into the myriad ways Artificial Intelligence is enhancing medical diagnosis, exploring the core technologies, practical applications, ethical considerations, and the exciting prospects that lie ahead for both clinicians and patients alike. We will uncover how AI is not just a technological advancement, but a paradigm shift, promising a new era of proactive, personalized, and ultimately, more precise healthcare.

The Diagnostic Imperative: Why Precision Matters More Than Ever
Accurate and timely diagnosis is the cornerstone of effective medical care. A misdiagnosis or a delayed diagnosis can have devastating consequences, leading to inappropriate treatments, prolonged suffering, increased healthcare costs, and, in severe cases, preventable mortality. Statistics paint a stark picture: diagnostic errors contribute to a significant number of adverse events in healthcare, underscoring an urgent need for improvement. The complexity of modern medicine, coupled with an aging global population and the rise of chronic diseases, places immense pressure on diagnostic systems.
The human element, while invaluable, comes with inherent limitations. Cognitive biases, fatigue, and the sheer volume of information a physician must process can all contribute to diagnostic challenges. Furthermore, access to specialized diagnostic expertise is often unevenly distributed, creating disparities in care. This global challenge necessitates innovative solutions that can augment human capabilities, standardize diagnostic processes, and make high-quality healthcare more accessible. The pursuit of diagnostic precision is no longer just an ideal; it is a critical imperative for the future of global health. AI offers a compelling pathway to address these systemic issues, promising to elevate diagnostic accuracy to unprecedented levels and usher in an era where every patient benefits from the most precise and timely insights available.

AI at the Forefront: Core Technologies Driving Diagnostic Transformation
The revolution in medical diagnosis powered by Artificial Intelligence is not driven by a single technology, but by a confluence of advanced computational techniques. These core AI technologies work in concert to process, analyze, and interpret vast quantities of medical data, enabling diagnostic breakthroughs that were once unimaginable. Understanding these foundational technologies is key to appreciating AI’s profound impact on healthcare.

Machine Learning (ML): The Engine of Predictive Analytics
Machine Learning, a subset of AI, involves algorithms that learn from data without being explicitly programmed. In medical diagnosis, ML models are trained on massive datasets of patient information—including symptoms, lab results, imaging data, and treatment outcomes—to identify patterns and make predictions. For example, an ML algorithm can learn to distinguish between benign and malignant tumors by analyzing thousands of pathology slides.
- Supervised Learning: This is the most common form in diagnostics, where models are trained on labeled data (e.g., images labeled as “cancer” or “no cancer”). The algorithm learns to map inputs to outputs, providing classifications or predictions.
- Unsupervised Learning: Used for finding hidden patterns or structures in unlabeled data, such as identifying new disease subtypes or patient cohorts with similar characteristics that might respond to specific treatments.
- Reinforcement Learning: While less common in direct diagnosis, it shows promise in optimizing treatment plans or guiding robotic surgery, where an agent learns through trial and error to achieve an objective.
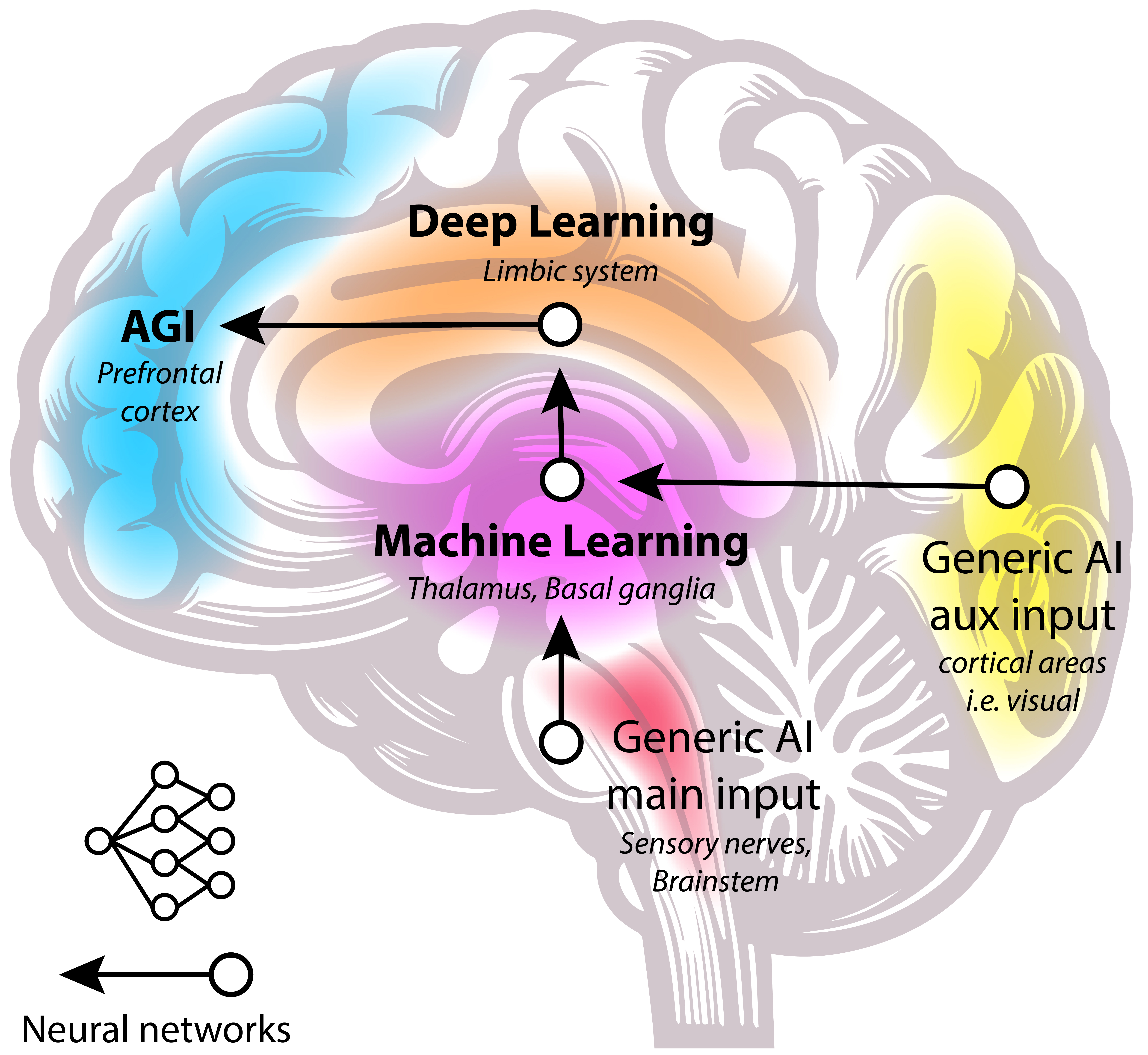
Deep Learning (DL): Mimicking the Human Brain for Complex Patterns
Deep Learning is a specialized branch of Machine Learning that uses artificial neural networks with multiple layers (hence “deep”) to learn representations of data with multiple levels of abstraction. Inspired by the structure and function of the human brain, deep learning algorithms are particularly adept at processing complex, high-dimensional data like medical images, genomics, and natural language.
- Convolutional Neural Networks (CNNs): These are the workhorses of medical image analysis. CNNs can automatically learn hierarchical features from raw image pixels, making them incredibly effective at tasks like detecting lesions, classifying diseases from X-rays, CTs, MRIs, and microscopic slides, and segmenting organs or abnormalities.
- Recurrent Neural Networks (RNNs): While less common for static images, RNNs, particularly LSTMs (Long Short-Term Memory networks), are excellent for sequential data like time-series physiological data (ECG, EEG) or electronic health record narratives, where the order of information is crucial.

Natural Language Processing (NLP): Unlocking Insights from Unstructured Text
Medical information is often stored in unstructured text formats, such as clinical notes, discharge summaries, pathology reports, and scientific literature. Natural Language Processing (NLP) is an AI field that enables computers to understand, interpret, and generate human language. In diagnostics, NLP is invaluable for:
- Extracting Key Information: Automatically identifying symptoms, diagnoses, medications, and procedures from free-text clinical notes.
- Synthesizing Patient Histories: Compiling comprehensive patient profiles from disparate textual sources, helping clinicians get a holistic view.
- Literature Review and Research: Rapidly sifting through vast amounts of medical literature to find relevant research, aiding in differential diagnosis and treatment planning.
By leveraging these powerful AI technologies, diagnostic systems can process information with unparalleled speed and accuracy, providing clinicians with invaluable insights to make more informed decisions. The synergy between these AI components forms the bedrock of the diagnostic transformation currently underway.
Revolutionizing Medical Imaging: Computer Vision’s Impact
Medical imaging—ranging from X-rays and CT scans to MRIs and microscopic pathology slides—is a cornerstone of modern diagnosis. However, interpreting these images requires immense expertise, is time-consuming, and can be subject to inter-observer variability. This is precisely where Computer Vision, a field of AI focused on enabling computers to “see” and interpret visual data, is making its most profound impact, transforming how diseases are detected and characterized.
AI in Radiology: Seeing Beyond the Human Eye
Radiologists are highly skilled professionals, but the sheer volume and complexity of images they review daily can lead to fatigue and potential oversight of subtle anomalies. AI-powered Computer Vision algorithms, particularly Deep Learning models like Convolutional Neural Networks (CNNs), are proving to be powerful allies.
- Automated Anomaly Detection: AI can rapidly scan X-rays, CTs, and MRIs to identify potential abnormalities such as tumors, fractures, or early signs of conditions like pneumonia or diabetic retinopathy. These systems can highlight suspicious areas, essentially acting as a “second pair of eyes,” prompting radiologists to review specific regions more closely. For example, AI algorithms have demonstrated high accuracy in detecting early-stage lung nodules on CT scans, often outperforming human radiologists in speed and consistency.
- Disease Classification and Quantification: Beyond detection, AI can classify diseases (e.g., differentiating types of brain tumors or identifying specific forms of arthritis) and quantify disease progression. In cardiac imaging, AI can precisely measure heart chamber volumes and ejection fractions, providing objective metrics for cardiovascular health.
- Streamlining Workflow: By prioritizing scans with critical findings or automatically segmenting organs, AI tools can significantly reduce the workload on radiologists, allowing them to focus on the most challenging cases and improve overall efficiency.
- Image Reconstruction and Enhancement: AI is also used to reconstruct clearer images from lower-quality or incomplete data, reducing scan times and patient exposure to radiation, especially in modalities like MRI and CT.
AI in Pathology: Microscopic Precision at Scale
Pathology involves the microscopic examination of tissue samples to diagnose diseases, particularly cancer. This is a labor-intensive process, and pathologists often review hundreds of slides daily. AI is poised to revolutionize this field, enhancing precision and throughput.
- Automated Cancer Detection and Grading: Deep learning algorithms can analyze whole-slide images (digitized microscope slides) to detect cancer cells, identify specific cancerous patterns, and even grade the aggressiveness of tumors (e.g., Gleason score for prostate cancer). This not only speeds up diagnosis but also reduces inter-pathologist variability.
- Biomarker Discovery: AI can identify subtle morphological features or patterns in tissue that correlate with specific genetic mutations or treatment responses, leading to the discovery of new diagnostic biomarkers.
- Quantitative Analysis: AI can quantify cellular features, mitotic activity, and tumor-infiltrating lymphocytes with high precision, providing objective data that supports diagnostic decisions and prognostic assessments.
- Quality Control: AI systems can act as a quality control mechanism, flagging slides that might have processing artifacts or areas that require re-examination, ensuring the highest diagnostic standards.
The integration of AI in medical imaging represents a monumental leap forward in diagnostic capability. By augmenting human expertise with machine precision and speed, Computer Vision is not just enhancing accuracy but also democratizing access to high-quality diagnostic interpretations globally.
Unlocking Insights from Data: Machine Learning in Clinical Decision Support
Beyond image analysis, a vast trove of diagnostic information resides within patient data, including electronic health records (EHRs), laboratory results, genomic sequences, and even wearable device data. Machine Learning (ML) is uniquely positioned to synthesize this diverse, complex, and often disparate information, transforming it into actionable insights that power Clinical Decision Support Systems (CDSS). These AI-driven tools assist clinicians in making more informed, personalized, and precise diagnostic and treatment decisions.
AI’s Role in Analyzing Electronic Health Records (EHRs)
EHRs contain a wealth of longitudinal patient data, but extracting meaningful insights from these often unstructured and voluminous records can be challenging for human clinicians. ML algorithms excel at this task:
- Identifying Risk Factors and Predicting Disease Onset: By analyzing historical EHR data, ML models can identify complex patterns and correlations that predict a patient’s risk of developing certain diseases (e.g., diabetes, cardiovascular disease, sepsis) even before symptoms manifest. This allows for proactive interventions.
- Differential Diagnosis Assistance: When a patient presents with a set of symptoms, an ML-powered CDSS can rapidly sift through millions of similar patient cases and medical literature to suggest a ranked list of potential diagnoses, along with the evidence supporting each. This significantly broadens the diagnostic possibilities considered by the clinician.
- Personalized Treatment Recommendations: ML can analyze a patient’s unique profile—including genetics, comorbidities, medication history, and past treatment responses—to recommend the most effective and safest treatment pathways, moving healthcare towards true precision medicine. For instance, in oncology, AI can match specific tumor mutations to targeted therapies with higher success rates.
- Medication Management and Adverse Event Prediction: AI can flag potential drug-drug interactions, adverse drug reactions, or non-adherence patterns by analyzing medication lists and patient notes, enhancing patient safety.
Leveraging Genomic and Multi-Omics Data for Precision Diagnostics
The advent of affordable genomic sequencing has opened new frontiers in personalized medicine. However, interpreting the vast amount of data from a patient’s genome, proteome, or metabolome requires sophisticated computational tools.
- Identifying Genetic Predispositions: ML algorithms can analyze an individual’s genetic variations to identify predispositions to specific diseases (e.g., certain cancers, autoimmune conditions) or predict their response to particular drugs (pharmacogenomics).
- Diagnosing Rare Diseases: For patients with rare or undiagnosed diseases, ML can compare their genomic profile and clinical symptoms against databases of known genetic disorders, significantly accelerating diagnosis and reducing the “diagnostic odyssey.”
- Biomarker Discovery and Validation: ML can sift through multi-omics data (genomics, proteomics, metabolomics) to discover novel biomarkers for early disease detection, prognosis, and therapeutic response, moving beyond traditional diagnostic markers.
Integrating Wearable Device Data for Continuous Monitoring
Wearable health devices generate continuous streams of physiological data (heart rate, activity levels, sleep patterns, blood glucose). ML models can process this real-time data to:
- Detect Early Warning Signs: Identify subtle changes in physiological parameters that might indicate the onset of an acute event (e.g., atrial fibrillation, impending heart attack) or the exacerbation of a chronic condition.
- Monitor Disease Progression: Provide continuous feedback on how a patient is responding to treatment or how a chronic disease is progressing, allowing for timely adjustments to care plans.
By integrating and interpreting diverse data sources, Machine Learning transforms raw information into actionable clinical intelligence. This empowers healthcare providers with unprecedented diagnostic support, leading to more accurate diagnoses, personalized treatment strategies, and ultimately, better patient outcomes.







