Cancer remains a formidable global health challenge, with millions of lives affected each year. The prognosis for many cancers dramatically improves when detected in its earliest stages, making early and accurate diagnosis a critical frontier in oncology. Traditionally, early detection has relied on a combination of screening programs, imaging techniques, and pathological analyses, often limited by human interpretation, inter-observer variability, and the sheer volume of data. However, a profound shift is underway. Artificial intelligence (AI) is rapidly emerging as a game-changer, offering unprecedented capabilities to analyze vast datasets, identify subtle patterns, and significantly enhance the precision and efficiency of early cancer detection.
From scrutinizing intricate medical images to sifting through complex genomic data and even analyzing circulating tumor cells in liquid biopsies, AI applications are pushing the boundaries of what’s possible. This technological revolution promises to not only augment the capabilities of oncologists and radiologists but also to democratize access to advanced diagnostic tools, ultimately leading to earlier interventions and improved patient outcomes. This comprehensive guide delves into the transformative power of AI in oncology, exploring its diverse applications, the challenges it faces, and the promising future it heralds for the fight against cancer.

The Urgency and Impact of Early Cancer Detection
The stark reality of cancer survival rates is often directly linked to the stage at which the disease is diagnosed. For many cancers, detecting the malignancy before it has spread beyond its primary site can significantly increase the chances of successful treatment and long-term survival. For instance, the five-year survival rate for localized breast cancer is over 99%, but it drops to 31% if the cancer has metastasized. Similar trends are observed across various cancer types, underscoring the paramount importance of early detection strategies.
Early diagnosis not only improves survival rates but also reduces the invasiveness of necessary treatments, leading to fewer side effects, better quality of life for patients, and lower healthcare costs. It allows for more effective therapeutic interventions, often enabling less aggressive surgeries, targeted therapies, or even watchful waiting in certain low-risk cases. The traditional methods, while foundational, often face limitations such as:
- Subjectivity in interpretation: Human radiologists and pathologists can sometimes miss subtle anomalies or disagree on findings, leading to false positives or false negatives.
- High workload and burnout: The increasing volume of diagnostic tests can overwhelm healthcare professionals, leading to fatigue and potential errors.
- Limitations of current screening tools: Some screening methods have inherent sensitivity or specificity limitations, leading to unnecessary biopsies or missed cancers.
- Access disparities: Advanced diagnostic technologies and expert interpretation are not uniformly available globally, creating significant inequalities in cancer care.
- Process immense datasets: AI can analyze petabytes of medical images, genomic sequences, pathology slides, and patient records in a fraction of the time it would take human experts.
- Enhance accuracy and consistency: By learning from validated cases, AI models can achieve high levels of accuracy in identifying cancerous lesions, often surpassing human performance in specific tasks and providing consistent interpretations.
- Identify subtle biomarkers: AI can uncover novel disease markers from complex data, leading to earlier detection of cancer even before overt symptoms appear.
- Personalize risk assessment: Through predictive analytics, AI can assess individual patient risk profiles, guiding personalized screening strategies and preventive measures.
- Reduce inter-observer variability: AI provides objective, data-driven interpretations, minimizing discrepancies between different human experts.
- Improve workflow efficiency: Automating repetitive tasks allows healthcare professionals to focus on complex cases and patient interaction, reducing burnout and improving overall system efficiency.
- Mammography and Breast Cancer Screening: AI algorithms are being trained on millions of mammograms to detect microcalcifications, masses, and architectural distortions indicative of early breast cancer. Studies have shown AI to be as good as, or even better than, human radiologists in identifying suspicious lesions, reducing false positives, and potentially decreasing the workload for radiologists. Some AI systems can even predict a woman’s future risk of developing breast cancer based on her mammogram.
- Example: Companies like Google Health and Zebra Medical Vision have developed AI models that can accurately detect breast cancer from mammograms, sometimes outperforming human experts in terms of sensitivity and specificity.
- Internal Link Suggestion: Explore more about Understanding Machine Learning in Healthcare for a deeper dive into the underlying technology.
- Lung Cancer Screening (CT Scans): Low-dose computed tomography (LDCT) is effective for screening high-risk individuals for lung cancer. AI can analyze LDCT scans to identify and characterize lung nodules, differentiating between benign and malignant lesions with high accuracy. This can reduce the number of unnecessary follow-up scans and biopsies while ensuring that truly suspicious nodules are flagged early.
- External Link Suggestion: Learn more about the National Lung Screening Trial and its impact on early detection at National Cancer Institute.
- Prostate MRI Analysis: AI assists in analyzing multi-parametric MRI (mpMRI) scans of the prostate, helping to identify suspicious regions and grade prostate cancer more accurately. This aids in targeted biopsies and reduces the need for systematic, often uncomfortable, biopsies.
- Radiomics: Beyond just detecting visible lesions, AI-powered radiomics extracts a wealth of quantitative features from medical images that are not discernible to the human eye. These features can include texture, shape, and intensity variations within a tumor. AI algorithms can then use these radiomic features to predict tumor aggressiveness, treatment response, and even patient prognosis, moving beyond simple detection to deeper characterization.
- Actionable Advice: Integrating AI-powered image analysis tools into existing radiology workflows can significantly improve diagnostic throughput and accuracy, allowing radiologists to focus on complex cases requiring nuanced human judgment.
- Automated Slide Analysis: AI algorithms can quickly scan entire pathology slides, identify suspicious areas, count cells, and even grade tumors based on morphological features. This helps pathologists prioritize cases, reduce screening time, and ensure consistency in diagnosis.
- Tumor Subtyping and Grading: AI can assist in accurately classifying different cancer subtypes and assigning grades, which are crucial for determining prognosis and treatment strategies. For example, in breast cancer, AI can identify different molecular subtypes directly from H&E stained slides, which traditionally required additional, more expensive tests.
- Detection of Micrometastases: Detecting tiny clusters of cancer cells (micrometastases) in lymph nodes is critical for accurate staging. AI algorithms can be trained to spot these elusive cells with greater sensitivity than the human eye, improving staging accuracy and preventing under-treatment.
- Predicting Treatment Response: By analyzing the subtle patterns within tumor architecture and cellular morphology, AI can potentially predict how a patient will respond to specific therapies, enabling more personalized treatment plans.
- Example: IBM Watson Health’s Pathology AI has been explored for assisting pathologists in prostate cancer grading, demonstrating capabilities to match or exceed human performance.
- Detecting Circulating Tumor DNA (ctDNA): Cancer cells shed DNA into the bloodstream. AI algorithms can analyze complex sequencing data from ctDNA to detect minute cancer signals, distinguish them from normal DNA, and even pinpoint the tissue of origin. This is particularly valuable for early detection in high-risk individuals or for monitoring minimal residual disease after treatment.
- Analyzing Circulating Tumor Cells (CTCs): CTCs are rare cancer cells that detach from the primary tumor and enter the bloodstream. AI-powered image analysis can identify and characterize these cells from blood samples, providing insights into tumor biology and metastatic potential.
- Proteomic and Metabolomic Analysis: AI can analyze vast datasets of proteins (proteomics) and metabolites (metabolomics) in body fluids to identify novel biomarkers associated with early-stage cancer. These molecular signatures can serve as powerful diagnostic indicators long before a tumor becomes clinically apparent.
- Quotable Statement: “Liquid biopsies, powered by AI, represent a paradigm shift, allowing us to ‘see’ cancer at its earliest molecular whispers, long before it roars.”
- Internal Link Suggestion: Discover more about The Promise of Precision Medicine and how it’s changing healthcare.
- Identifying Genetic Predispositions: AI can analyze an individual’s germline DNA to identify genetic mutations or single nucleotide polymorphisms (SNPs) associated with an increased risk of developing certain cancers (e.g., BRCA1/2 for breast and ovarian cancer). This allows for proactive screening and preventive measures.
- Early Detection through Somatic Mutations: By analyzing somatic mutations (changes in tumor DNA), AI can help detect the presence of cancer, even in its very early stages, from biopsy samples or liquid biopsies. It can identify driver mutations that are characteristic of specific cancer types.
- Multi-omics Data Integration: The true power of AI lies in its ability to integrate and analyze data from multiple “omics” sources—genomics, transcriptomics, proteomics, metabolomics, and epigenomics. By finding correlations and patterns across these different layers of biological information, AI can construct a more comprehensive picture of disease, leading to more robust early detection markers and personalized risk stratification.
- Actionable Advice: For researchers, leveraging AI in multi-omics data analysis can accelerate the discovery of novel cancer biomarkers, moving from correlation to causation more efficiently.
These challenges highlight the urgent need for innovative solutions that can enhance the accuracy, efficiency, and accessibility of early cancer detection. This is precisely where AI, with its capacity for pattern recognition and data synthesis, steps in as a powerful ally.

How AI Transforms Cancer Diagnostics
Artificial intelligence, encompassing machine learning (ML) and deep learning (DL), is fundamentally changing how medical data is processed, interpreted, and utilized for diagnostic purposes. Unlike traditional rule-based programming, AI algorithms learn from vast amounts of data, identifying intricate patterns and relationships that are often imperceptible to the human eye or too complex for manual analysis. In cancer diagnostics, AI’s transformative power stems from its ability to:
Key takeaway: AI is not replacing oncologists but augmenting their capabilities, providing an invaluable second opinion and powerful analytical tools to elevate the standard of care.
The integration of AI in oncology is leading to an era of precision oncology, where diagnostic and treatment strategies are tailored to the individual characteristics of each patient’s cancer. This move away from a “one-size-fits-all” approach is crucial for improving outcomes and minimizing unnecessary interventions.
Specific AI Applications in Early Cancer Detection
AI’s versatility allows for its application across various modalities crucial for early cancer detection. Each area leverages AI’s strengths to overcome specific challenges and unlock new diagnostic possibilities.
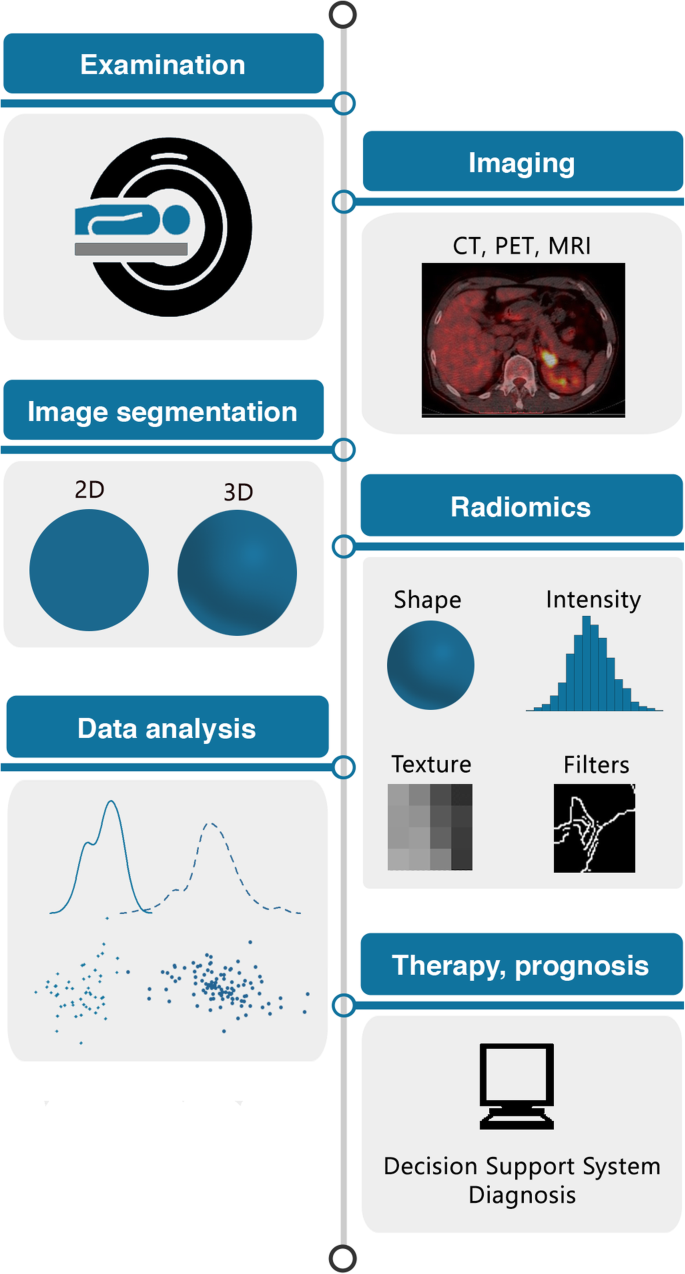
Image Analysis and Radiomics
Medical imaging—such as mammography, CT scans, MRIs, and ultrasounds—forms the cornerstone of cancer screening and diagnosis. However, interpreting these images is a highly specialized and time-consuming task, often prone to human error, especially when identifying subtle or early-stage lesions. This is where AI, particularly deep learning, shines.

Pathology and Histopathology
Pathology, the microscopic examination of tissue samples, is the gold standard for definitive cancer diagnosis. However, this process is labor-intensive, requires highly specialized expertise, and can be subjective. AI, particularly deep learning, is revolutionizing digital pathology by analyzing digitized whole-slide images (WSIs).
Liquid Biopsies and Biomarker Discovery
Liquid biopsies involve analyzing body fluids (like blood, urine, or saliva) for cancer-related biomarkers, such as circulating tumor DNA (ctDNA), circulating tumor cells (CTCs), or exosomes. This non-invasive approach holds immense promise for early detection, especially for cancers that are difficult to screen, and for monitoring disease recurrence. AI is indispensable in making sense of the incredibly complex and often low-abundance signals in liquid biopsies.
Genomic and Proteomic Analysis
The advent of next-generation sequencing has generated an explosion of genomic, transcriptomic, and proteomic data. This “omics” data contains a treasure trove of information about an individual’s cancer risk and the specific characteristics of their tumor. However, interpreting this high-dimensional data is a monumental task for humans. AI is uniquely positioned to unlock its secrets.
Risk Assessment and Predictive Modeling
Beyond direct detection, AI plays a crucial







